Suicidal Patient Refusing Treatment
Suicidal patient refusing treatment. Be sure you are a patient who is allowed to refuse medical treatment and that you are not in a category where the refusal is restricted. An hour later she arrives in the emergency department with a friend but refusing treatment saying she wishes to die. A 19 year old woman takes a potentially lethal overdose of paracetamol and amitriptyline.
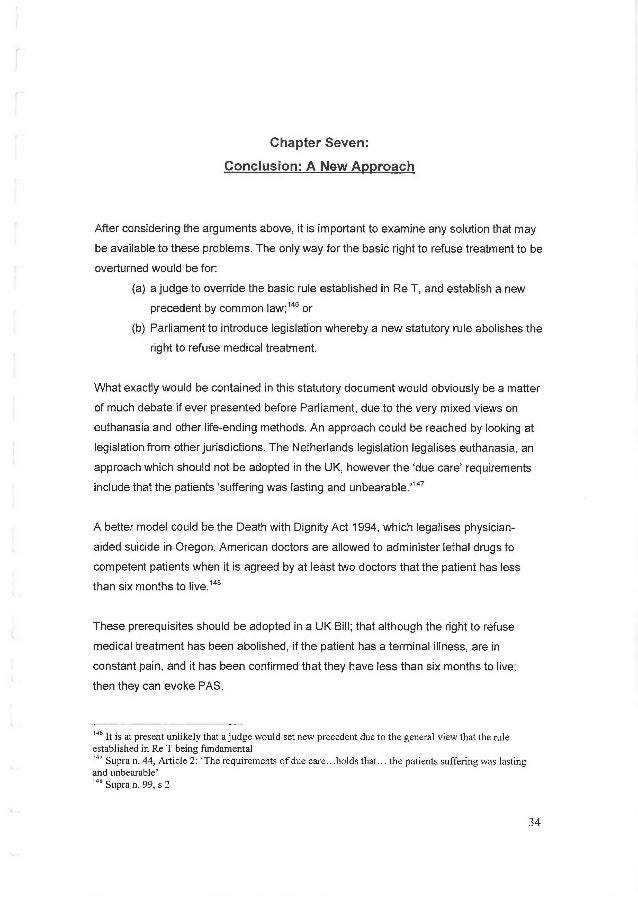
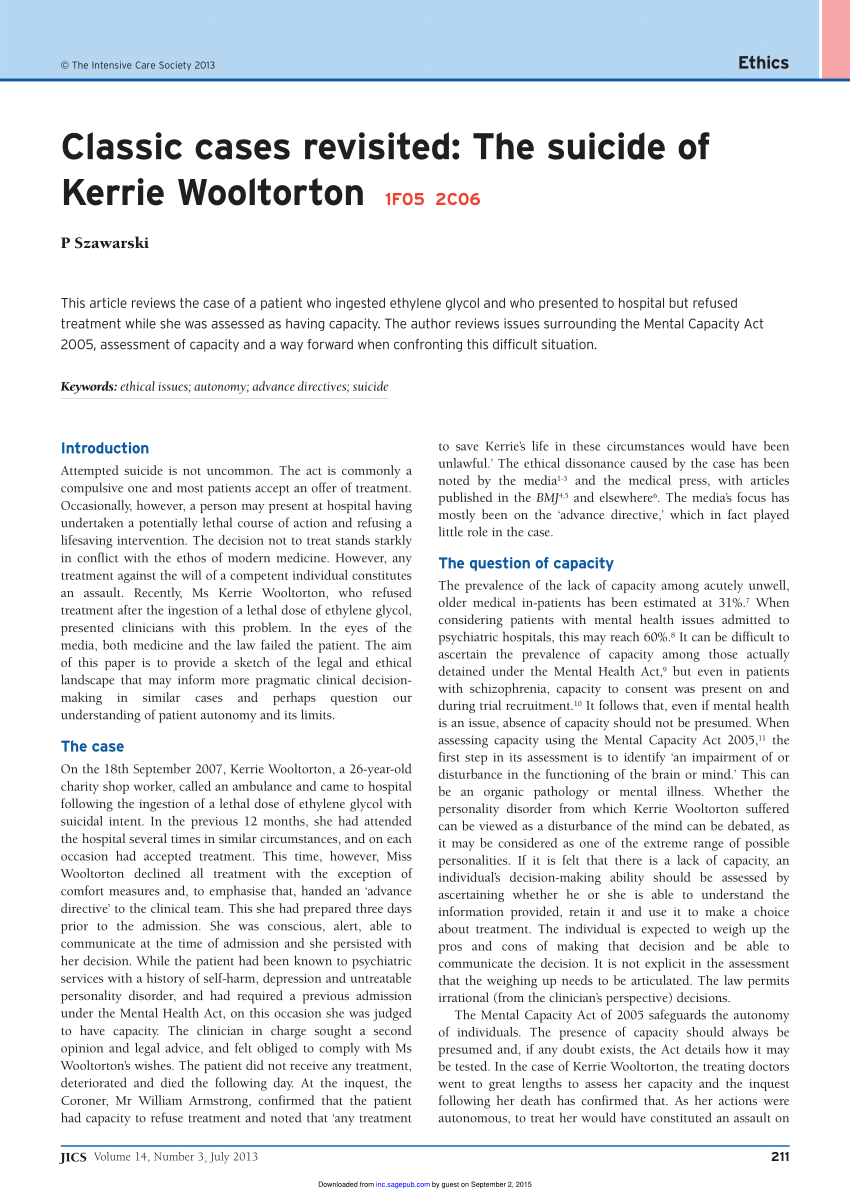
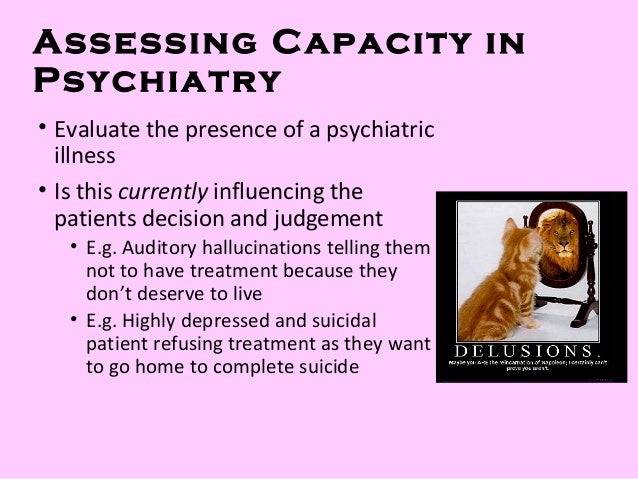
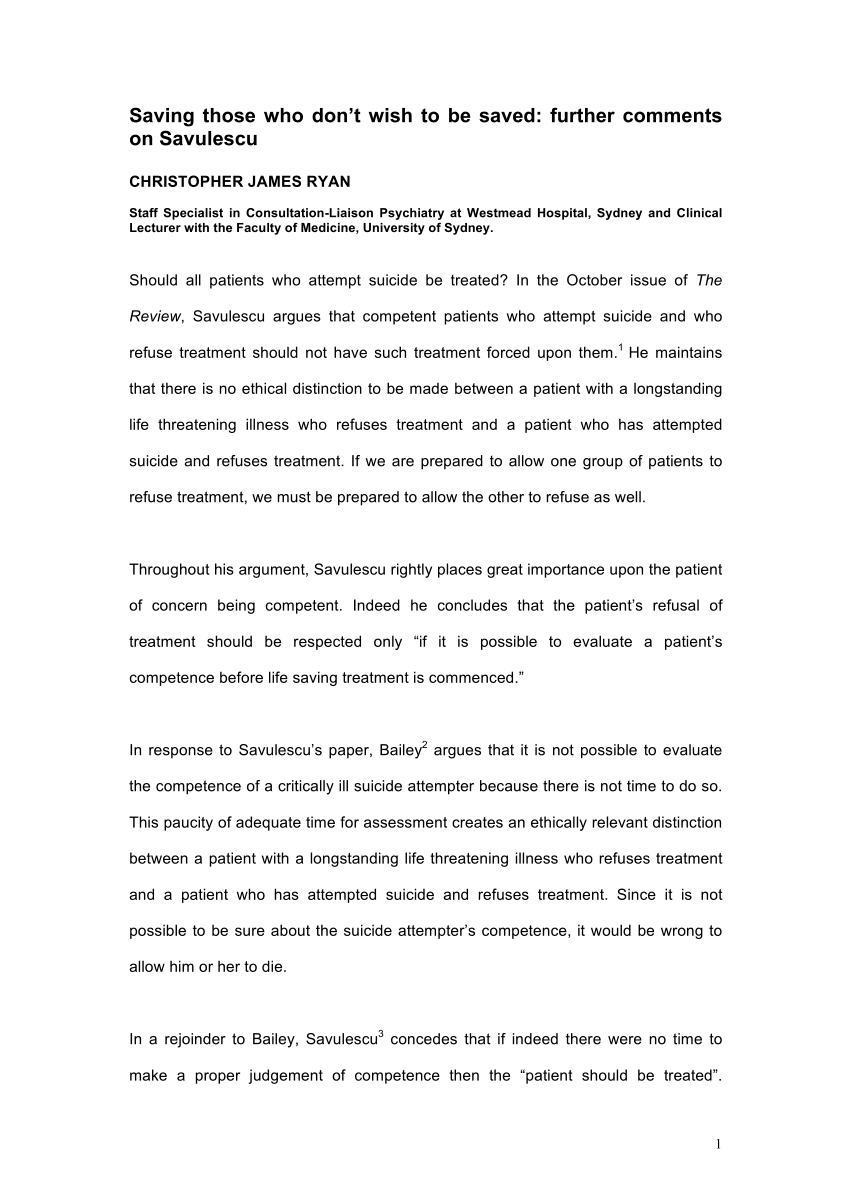
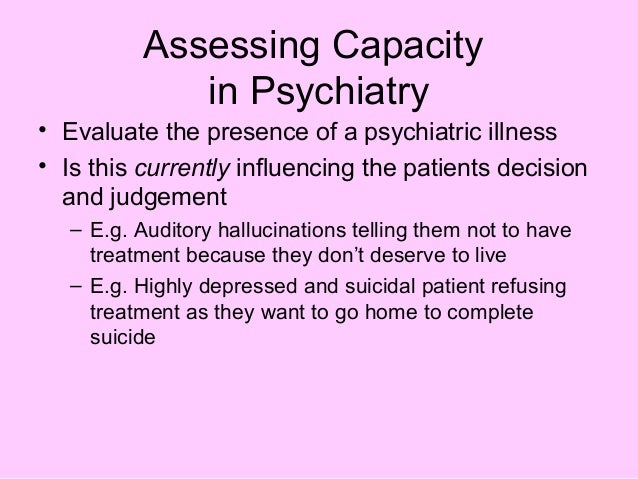
Rethinking Capacity and Coercive Treatment in Light of the Kerrie Wooltorton Case. If past treatment preferences cannot be established with sufficient certitude a therapeutic trial of treatment for the depression may be justified even if the patient currently refuses the treatment as in such circumstances the determination of competence during the depression may be possible only after successful treatment of the depression when it can be evaluated whether the treatment preferences. Assessment and treatment of underlying psychiatric conditions such as depression anxiety bipolar disorder and.
You have very little if anything usually available to legally prevent them from leaving. Clinicians should act with caution given the potential for recovery and fluctuations in suicidal ideation. For the suicidal patient thats not on a hold thats alert and oriented thats not combative if the patient wants to leave so be it.
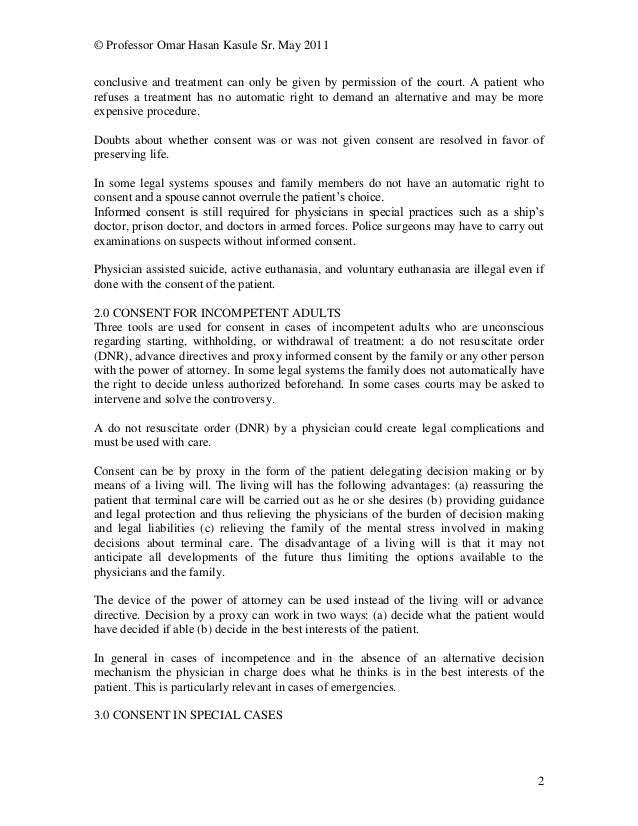
When it is not possible or is inappropriate to treat under mental. Legal and ethical aspects of refusing medical treatment after a suicide attempt. A patient who is suffering a terminal illness who takes an active step to end their own life in advance of death being caused by the illness is committing suicide.
Refusing Medical Treatment After Attempted Suicide. If your loved one refuses to move forward its useful to try to understand what is behind his reasons for refusing treatment and then address those issues. A person may refuse to accept mental.
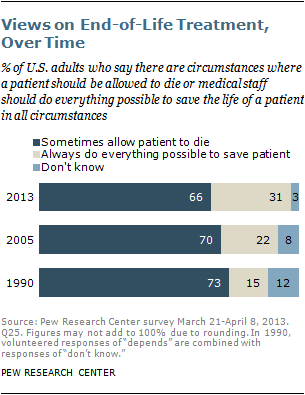
Increasingly patients are exercising the right to refuse treatment. Sent to emergency physicians around Trent asking for their reaction 1. There are exceptions to a patients right to refuse treatment.
About 30 of acute medical inpatients lack capacity to make key decisions about their treatment1 and this rises to above 40 for psychiatric inpatients2 Clinicians tend to overestimate patients capacity and miss cases where capacity is lacking3 Navigating the relevant legal frameworks common law the Mental Capacity Act MCA and the Mental Health Act MHA can seem daunting. A patient who declines medical treatment for a terminal illness knowing that the illness will lead to death dies of natural causes.
The majority of suicidal ED patients however do need a comprehensive risk assessment to inform decisionmaking about treatment and disposition.
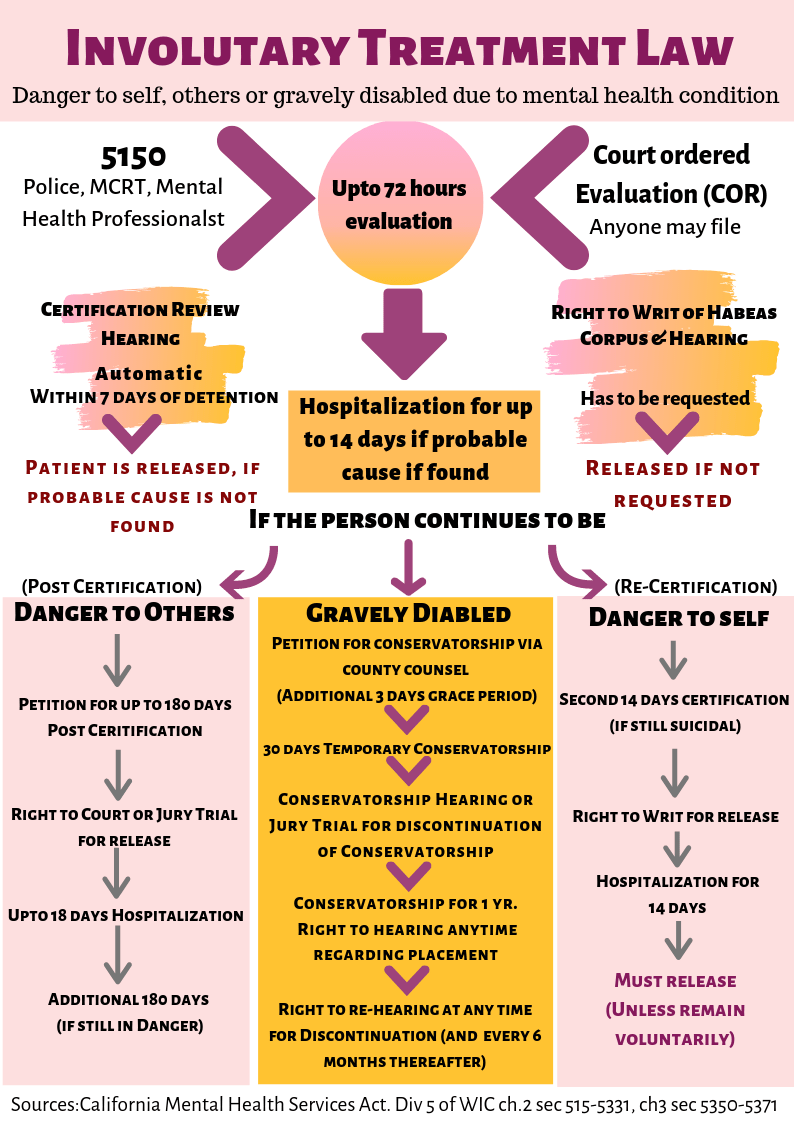
A doctor may provide involuntary treatment usually a medication given by injection or by mouth but only to control the emergencywhich again is defined as an imminent danger to self or others. When it is not possible or is inappropriate to treat under mental. If your loved one refuses to move forward its useful to try to understand what is behind his reasons for refusing treatment and then address those issues. The legal and bioethics literature on competence to refuse lifesaving treatment and the possible impact of depression on this refusal is. A doctor may provide involuntary treatment usually a medication given by injection or by mouth but only to control the emergencywhich again is defined as an imminent danger to self or others. There are exceptions to a patients right to refuse treatment. An hour later she arrives in the emergency department with a friend but refusing treatment saying she wishes to die. For an adequate risk assessment the patient should be cognitively able to participate. In an emergency all bets are off.
Be sure you are a patient who is allowed to refuse medical treatment and that you are not in a category where the refusal is restricted. Four specific treatment options have proven especially helpful. If past treatment preferences cannot be established with sufficient certitude a therapeutic trial of treatment for the depression may be justified even if the patient currently refuses the treatment as in such circumstances the determination of competence during the depression may be possible only after successful treatment of the depression when it can be evaluated whether the treatment preferences. For the suicidal patient thats not on a hold thats alert and oriented thats not combative if the patient wants to leave so be it. Dialectical Behavioral Therapy is heavily based on the same principles as CBT but instead uses acceptance and coming to terms with chronic negative thoughts and behaviors and uses that as a foundation to build balance and make positive change seem possible. The legal and bioethics literature on competence to refuse lifesaving treatment and the possible impact of depression on this refusal is. Clinicians should act with caution given the potential for recovery and fluctuations in suicidal ideation.









/GettyImages-1059416456-15160a7b08f7489baae2a196530e022b.jpg)


/GettyImages-106914481-568586f33df78ccc15e548e5.jpg)




/committed-against-my-will-56af37a75f9b58b7d0160eae.jpg)






Posting Komentar untuk "Suicidal Patient Refusing Treatment"